NexBioHealth is privileged to feature Dr. Thiruvengadam Muniraj, a distinguished advanced endoscopist and leader in pancreatic and bariatric endoscopy at Yale University. As an International Medical Graduate with a remarkable journey from India to the U.S., Dr. Muniraj exemplifies excellence, resilience, and innovation in medicine. We interviewed him to explore his inspiring career path, his groundbreaking contributions to advanced endoscopy, and his advice for young physicians navigating the evolving landscape of healthcare.
- April 1, 2024
Kyoung Ryul Lee, MD, PhD, CEO of the SCL Group, Seoul Clinical Laboratory, a Specialist in Laboratory Medicine
Kyoung Ryul Lee, MD, PhD, CEO of the SCL Group, Seoul Clinical Laboratory, a Specialist in Laboratory Medicine What motivated your decision to attend medical school and become a physician? Could you share some particularly
- August 5, 2024
ISSUE 28
FROM THE PUBLISHER W elcome to the 28th edition of the World Asian Medical Journal. This issue encompasses a captivating cover story featuring an interview with Dr. Huang, a distinguished medical professional whose journey from
- August 5, 2024
Youngmee Jee, MD, PhD | Inspirational Asian Healthcare Leader
INSPIRATIONAL ASIAN HEALTHCARE LEADER Youngmee Jee, MD, PhD Commissioner of Korea Disease Control and Prevention Agency INTERVIEW 01 Tell us how you decided to pursue a career in medicine. How did you choose your specialty?
- September 21, 2024
Rethinking Hypothyroidism
Rethinking Hypothyroidism: Why Treatment Must Change and What Patients Can Do Author: Antonio C. Bianco, MD Translated by: Semin Kim, MD & Sihoon Lee, MD About the book “Rethinking Hypothyroidism” The limitations of current
- October 1, 2024
The Internet of Things (Revision 2021)
Purchase LinkThe Internet of Things (Revision 2021) Author: Sam Greengard We turn on the lights in our house from a desk in an office miles away. Our refrigerator alerts us to buy milk on the
- October 1, 2024
Superconvergence
Purchase LinkSuperconvergence Author: Jamie Metzl In Superconvergence, leading futurist and OneShared World founder Jamie Metzl explores how artificial intelligence, genome sequencing, gene editing, and other revolutionary technologies are transforming our lives, world, and future. These
- October 12, 2024
The Strategic Importance of Location in the U.S. for Foreign Bio and Pharma Companies
The Strategic Importance of Location in the U.S. for Foreign Bio and Pharma Companies DoHyun Cho, PhD (CEO, W Medical Strategy Group) The U.S. Market: A Cornerstone of Global Expansion For pharmaceutical and biotech companies,
- October 12, 2024
South Korea’s Healthcare Crisis: Beyond the Numbers
South Korea’s Healthcare Crisis: Beyond the Numbers Dongju Shin, Dong-Jin Shin INTRODUCTION The South Korean healthcare system has recently plunged into a significant crisis following a February 2024 announcement by the government to increase medical
- October 14, 2024
Overcoming Disparities in Gastric Cancer Care
Overcoming Disparities in Gastric Cancer Care Chul S. Hyun, MD, PhD, MPH Gastric Cancer and Prevention Screening Program, Yale School of Medicine, New Haven, CT Gastric cancer is the fifth most common cancer worldwide,
- October 15, 2024
The Global OR – An Introduction to Global Surgery
The Global OR – An Introduction to Global Surgery Kee B. Park, MD, MPH, Dawn Poh, MBBS, MRes Introduction An estimated 5 billion people worldwide lack access to timely, affordable, and safe surgical care, including
- February 1, 2025
- Journey in Medicine
India to the US
Q&A
How did your upbringing in India shape your career in medicine, and what values or experiences have stayed with you throughout your journey?
I grew up in Tamil Nadu, South India, where our home was part of an agricultural community. Life was simple and profoundly connected with nature, with the sounds of roosters greeting us each morning and cattle living in the same space as the family. My days often began before sunrise, accompanying my paternal grandfather to our farmland before school. We’d walk the fields together, observing the crops, discussing irrigation, and managing farm workers. What seemed like ordinary early morning chores at the time were actually lessons —they were a masterclass in responsibility, patience, and leadership. Through those routines, I learned that nurturing—whether it’s a crop, a team, or later, a patient—requires effort, focus, and care.
As the eldest grandchild among more than a dozen cousins, I often accompanied my grandfathers. My maternal grandfather, a cotton merchant, taught me humility and generosity through his business dealings, earning trust and respect. In contrast, my paternal grandfather, a farmer, demonstrated resilience and resolve at farmers’ markets, negotiating prices with confidence. Their differing styles shaped my approach to leadership—balancing empathy with strength, and listening with conviction Both men left profound imprints on my life. My maternal grandfather, despite his third-grade education, was one of the wisest people I knew, raising seven children and sponsoring others’ education. His philosophy, “It’s a privilege to help someone,” became my guiding principle. My paternal grandfather, who farmed until 98 and lived to 100, embodied resilience in a rain-dependent agricultural community, teaching me perseverance through unpredictability.
My mother, meanwhile, was a quiet yet unshakable force. A working woman balancing career and family, she instilled in me the value of hard work and the unseen sacrifices of those who support us. Her dedication ensured I had the tools to succeed, reminding me that success is built on both talent and effort.
Early Leadership Lessons in Medicine
In my early career, I found myself thrust into a leadership role at a hospital in Coimbatore, the city where I grew up. The institution was struggling financially, and when its owner relocated to England, I was entrusted with managing both clinical and administrative responsibilities. Balancing the demands of patient care with the complexities of running a healthcare facility was a time of immense personal and professional growth. As an administrator, I was treated with deference and given special complaisance, not for who I was but because of the position I held. When the hospital was sold, and I returned as a clinician without administrative responsibilities, the dynamic changed dramatically—the privileges disappeared, and I was just another doctor in the halls. That experience was humbling and taught me a powerful lesson: the respect and attention tied to a position are fleeting and belong to the role, not the individual. True respect comes from character and actions, not titles or status. This realization strengthened my resolve to stay grounded and to always be ready to return to basics.
Being Tamil and What It Taught Me
Growing up, Tamil culture deeply shaped my identity and continues to guide me. In Tamil Nadu, hospitality is a cornerstone of daily life, epitomized by the heartfelt question, “Have you eaten?” (or “Saapittingala?”). This goes beyond a casual greeting; it’s a genuine expression of care, reflecting a belief that no one should go hungry. Offering food or checking on someone’s meal embodies a warmth that transcends social barriers, making everyone feel welcomed. This cultural value has profoundly influenced my approach to patient care. Small gestures, like ensuring a patient’s comfort or asking if she needs assistance, mirror the spirit of Tamil hospitality, fostering trust and connection.
Even in professional settings far from Tamil Nadu, this deeply ingrained habit of genuine concern continues to shape my interactions. Whether offering a kind word to a colleague, checking on a patient’s comfort, or simply asking if I can get someone a coffee, this caring instinct remains a guiding principle. It’s a quiet but powerful reflection of Tamil culture, one that I carry with me wherever I go, reminding me that true connection begins with small, sincere acts of care.
Can you describe your transition from practicing medicine in India to the U.S.? What were the biggest challenges, both culturally and professionally, and how did you overcome them?
Most IMGs will have experiences similar to mine. The journey from practicing medicine in India to the U.S. was a transformative experience, filled with challenges, surprises, and moments of deep reflection. Each phase of my career— from my early days in an overcrowded government hospital in Tamil Nadu to rural private practice, from working in the Sultanate of Oman to navigating the U.S. healthcare system— has shaped how I see medicine and the world.
Practicing Medicine in India: Resourcefulness in Chaos
I began my training at a government hospital affiliated with Coimbatore Medical College, one of the busiest institutions in the region. The hospital often operated at five times its capacity. Patients filled every bed, lined the floors, and spilled into the corridors. I remember seeing entire families camping in the hallways to stay close to their loved ones. Despite the overwhelming numbers and limited resources, we made it work. We relied heavily on quick thinking, collaboration, triaging, and resource allocation to prioritize care. It was a constant balancing act, but those early days taught me how to make decisions under pressure, maximize the tools at hand, and work as a team to provide the best possible outcomes. There wasn’t the luxury of advanced imaging or a plethora of medications, but what we lacked in technology, we made up for in ingenuity and dedication. In 1997, I started my own private practice in Thekkalur, a rural village in Tamil Nadu, India. This was a different world entirely. Instead of the chaos of a government hospital, I had a more intimate connection with my patients in this close- knit community. I could take the time to hear their stories, understand their lives, and be part of their journey to recovery. I quickly realized that one of the most rewarding aspects of medicine is the feedback patients give —a smile, a heartfelt thank you, or the trust they place in you and often gifts in the form of farm produce. It was a reminder that medicine isn’t just about diagnosing and treating; it’s about building trust and being a part of people’s lives. It’s a privilege I carry with me to this day.
Practicing Medicine in Oman: Medicine Without Borders

After years in India, I moved to the Sultanate of Oman to work in a completely new cultural environment. Practicing medicine in an Arabic country was eye-opening in many ways. Patients and families in Oman had a profound respect for doctors but care often had to align with cultural and religious values. Decisions were often a family affair, requiring me to carefully balance modern medical practices with traditions and beliefs. At first, it was daunting—I didn’t speak Arabic, and I wasn’t familiar with the cultural nuances. But I immersed myself in the environment, slowly learning the language and understanding the local customs and culture. I learned that the universal language of empathy and care could bridge almost any gap. Patients everywhere want the same things: to feel heard, understood, and cared for. While Oman had better resources than the government hospital in India, the emphasis was still on the human connection, and that resonated with me. My time there reinforced that medicine is universal, even if the context changes. Whether it’s a family in Oman seeking reassurance through faith or a patient in India looking for hope in a crowded ward, at the core, people are the same.
One of the most memorable aspects of this role was supporting American troops stationed in the Omani desert, providing medical resources to their units. It was a unique experience that broadened my perspective on healthcare beyond cultural and geographical boundaries. Later, when I moved to the US, I received a letter of recommendation from a U.S. military commander for my efforts, which proved invaluable when I applied for permanent residency in the U.S., expediting my green card process. It was one of those moments that reminded you how the dots in life connect in ways you never anticipate—proof that every step has a purpose, even if you don’t see it right away.
Transitioning to the U.S.: Adapting to a New System
Moving to the U.S. brought both opportunities and challenges. The system offered cutting-edge technology, structured workflows, and access to advancements I had only dreamed of. Adapting to its bureaucratic complexity, however—insurance, documentation, and administrative layers—was overwhelming. In India and Oman, physicians had more autonomy, whereas U.S. medicine emphasized team-based, protocol-driven care. This collaborative approach required adjusting my decision- making style and embracing structure.
The patient-doctor dynamic also differed. In India and Oman, patients deferred to doctors, while in the U.S., they are informed and actively engaged, fostering a deeper partnership through clear communication and education. The U.S.’s cultural diversity was both enriching and challenging. My experience in Oman had prepared me to approach care with cultural sensitivity and adaptability, skills that proved invaluable in navigating this new environment.
Challenges and Lessons Along the Way
Navigating the complexities of medicine in the U.S. presented new challenges, particularly in managing administrative hurdles such as insurance approvals and billing—issues rarely encountered in India. Each phase of my career— India, Oman, and the U.S.—offered invaluable lessons. From India, I learned resourcefulness and the art of doing the best with limited resources. Oman taught me the significance of cultural understanding and respect in building trust. The U.S. emphasized the importance of structure, teamwork, and patient-centered care. Ultimately, the most profound realization across all these experiences was that medicine transcends treating diseases; it is about understanding and connecting with people.
Coming to the US was never a part of my dream when I was in India. From walking the crowded wards of a government hospital in India to supporting American troops in Oman to practicing medicine in the U.S., each step has been a building block for the next. I often think of the letter from the U.S. military commander in Oman that helped expedite my green card. As Steve Jobs famously said, “You can’t connect the dots looking forward; you can only connect them looking backward.”
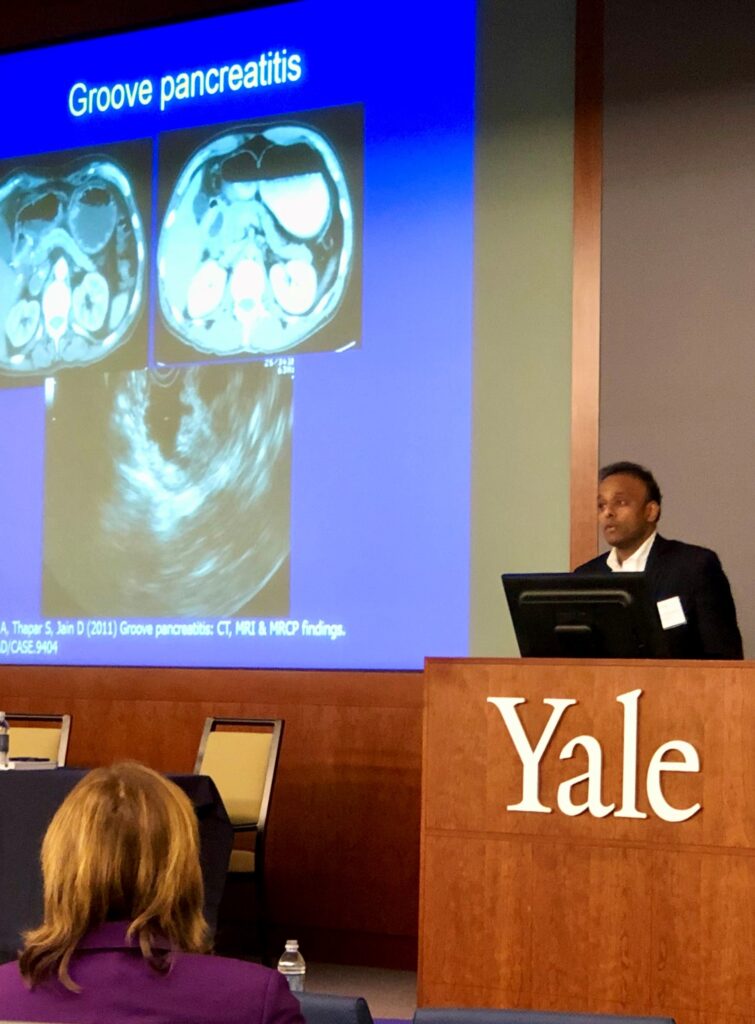
You’ve introduced several novel endoscopic procedures in Connecticut. Could you highlight one or two that had the most significant impact on patient care?

One of the most fulfilling aspects of my work at Yale has been pioneering several of the first-ever advanced endoscopic procedures in Connecticut, transforming care for patients with complex gastrointestinal conditions. For patients with Roux-en-Y gastric bypass (RYGB), whose altered anatomy makes traditional ERCP nearly impossible, I introduced the EDGE procedure (EUS (endoscopic ultrasound) -guided ERCP). This innovative approach eliminates the need for complex surgery, providing a safe, minimally invasive pathway to the biliary system, reducing recovery time, and offering new hope to patients with limited options. Another impactful advancement is EUS-guided interventions such as pancreatic necrosectomy, duct/lumen anastomoses and drainage. These techniques allow us to connect the pancreatic duct, bile duct, or small bowel to the stomach, perform gallbladder drainage for cholecystitis, and manage severe necrotizing pancreatitis—all without traditional surgery. These procedures have been transformative for high-risk patients, offering faster recoveries and fewer complications. Witnessing the profound improvement in patients’ quality of life through these innovations is the most rewarding part of my work.
What drives your passion for advancing techniques and technologies in interventional endoscopy?
As mentioned earlier, my journey began during my medical training in India. Limited resources and overwhelming patient volumes taught me to think creatively, prioritize under pressure, and connect deeply with underserved communities. These experiences shaped my belief that medicine is not just about treating illness but innovating to improve care, even in challenging circumstances. This drive to push boundaries has remained constant throughout my career.
Today, with access to cutting-edge technologies in the U.S., my mission remains focused on improving patient outcomes while minimizing the physical and emotional toll of treatment. Offering less invasive, more effective solutions and witnessing patients recover faster and regain their quality of life is the most rewarding part of my work.
Interventional endoscopy thrives on curiosity and collaboration. I’m fortunate to work with four exceptionally talented advanced endoscopy partners who share a vision for advancing care. Together, we explore new techniques and integrate emerging technologies to meet the evolving needs of our patients. Every innovation represents an opportunity to reduce suffering and provide transformative care—an unwavering mission that began in India and continues in Connecticut.
As Clinical Chief for Endoscopy at Yale, how do you mentor and support aspiring physicians, particularly IMGs?
Mentoring the next generation of physicians, including IMGs, is one of the most fulfilling parts of my role at Yale. Having started my medical journey in India and navigated the challenges of transitioning across continents, I deeply relate to the hurdles IMGs face in adapting to new healthcare systems. Their passion, curiosity, and drive remind me of my own journey and inspire me to guide them.
I provide tailored mentorship, from collaborating on research projects to offering insights and advice through regular calls, often during weekends. I aim to help IMGs integrate into the U.S. healthcare system while embracing their unique strengths. Through Yale’s IMG electives, I’ve connected with many talented candidates and remain invested in their progress. Watching them evolve and succeed motivates me to continually refine my own teaching and leadership, ensuring I provide the best possible guidance.
What is your vision for the future of interventional endoscopy and digestive health, especially in bariatric endoscopy? How do you see your work at Yale shaping the next generation of physicians and advancing the field of gastroenterology?
My vision for Yale Interventional Endoscopy is to transform digestive health through innovative, minimally invasive solutions, establishing our program as a national leader in advanced endoscopy not only in the Northeast but in the entire USA. Bariatric endoscopy, in particular, holds immense potential to combat obesity and its comorbidities. The rise of GLP-1 receptor agonists has revolutionized care, creating opportunities to integrate endoscopic therapies such as endoscopic sleeve gastroplasty (ESG) as complementary or alternative treatments, offering safer, less invasive options for
surgery. Refining these techniques will enhance outcomes and accessibility for patients. As Clinical Chief for Endoscopy, I am equally committed to cultivating the next generation of gastroenterologists. At Yale, we train advanced endoscopy fellows, immersing them in cutting-edge procedures and research. Beyond technical skills, I emphasize empathy, adaptability, and innovation, preparing fellows to address the diverse and evolving needs of patients. The passion and fresh ideas of young trainees inspire me to continue pushing boundaries and fostering transformative care.
Interventional endoscopy is at a pivotal moment, offering solutions that reduce the need for surgery, improve outcomes, and expand access. My goal is to ensure Yale remains at the forefront of this transformative field, driving innovation and shaping the future of gastroenterology.
Looking back on your journey, what pivotal moments or decisions shaped your career, and what advice would you offer to IMGs aspiring to establish themselves in the U.S. healthcare system?
Starting a rural private practice in India, moving to Oman, and transitioning to the U.S. were transformative milestones. Each step taught me resilience, cultural sensitivity, and the value of service. For instance, a recommendation from a U.S. military commander for my work in Oman expedited my green card, underscoring how life’s dots connect in unforeseen ways. These experiences solidified my belief that medicine is fundamentally about people and connections, not just tools or techniques.
To IMGs, I would say: be resilient and adaptable. Focus on excelling in USMLE exams, gaining U.S. clinical experience, and building strong professional relationships. Highlight your global perspective as an asset, seek mentors who understand your journey, and embrace constructive feedback. With persistence and a growth mindset, you can navigate challenges, thrive, and make a meaningful impact in the U.S. healthcare system.
What message would you like to share with the readers of NexBioHealth about the importance of diversity, inclusion, and the role of IMGs in advancing U.S. medicine and healthcare?
I’ve witnessed it firsthand: the spark in a patient’s eyes when she feels truly understood, when her language is spoken, and her culture is respected. IMGs bring resilience, global perspectives, and cultural competence, enriching patient care and creating deeper, more meaningful connections. Diversity isn’t just a value—it’s a catalyst for innovation and a cornerstone of empathy in medicine.
NexBioHealth’s mission to empower young physicians aligns seamlessly with this vision. By showcasing the stories, achievements, and challenges of IMGs, the magazine amplifies diverse voices and promotes collaboration. It’s not merely about representation; it’s about inspiring and equipping the next generation of physicians with the tools to lead in an increasingly interconnected and globalized healthcare landscape.

Thiruvengadam Muniraj, MD, FACG, FRCP
Associate Professor of Medicine (Digestive Diseases)
Vice-Chief (Endoscopy), Digestive Diseases; Director of Advanced Endoscopy, YNHHS; Associate Chief of Endoscopy, Digestive Health; Director, Yale Center for Pancreatitis; Director, Bariatric Endoscopy
Dr. Muniraj serves as the Clinical Chief for Endoscopy at Yale University School of Medicine and the Associate Chief for Digestive Health at Yale New Haven Health. He leads groundbreaking programs in advanced and bariatric endoscopy, introducing innovative procedures such like EUS-based gastrojejunostomy and advanced ERCP techniques, positioning Yale as a leader in the field.
A top graduate of Coimbatore Medical College, India, Dr. Muniraj served as an assistant professor of medicine and hospital executive in India and Oman before moving to the U.S., where he completed internal medicine training at the University of Pittsburgh and a gastroenterology fellowship at Yale, earning the prestigious Samuel Kushlan Award.
As a respected researcher, author, and educator, Dr. Muniraj has numerous publications and is a frequent speaker at international conferences. He is the Associate Editor of Gastrointestinal Endoscopy and a Fellow of the Royal College of Physicians, London. His career exemplifies the vital contributions of International Medical Graduates to advancing global healthcare and medical innovation.